Clinical pharmacology support studies routinely required for IMP registration.
- Darren Wogman
- Apr 25, 2021
- 19 min read
Updated: May 25, 2021
Describe the clinical pharmacology support studies that are routinely required for the registration of a small molecule drug. You should cover the rationale, objectives and design of each study, and you should critically evaluate how the data are used to support prescribing statements, illustrate your answer with specific examples from Summaries of Product Characteristics (SmPC).
An assignment by: Darren Wogman MSc. Completed as part of Pharmaceutical Medicine MSc at King's College London
Introduction
The Summary of Product Characteristics (SmPC) is legally required by regulatory agencies. In the USA, the SmPC is referred to as the ‘Prescribing Information’ in either case, it is a dynamic document updated throughout the life-cycle of a drug, as new data emerges from the reporting of adverse effects and clinical practice. It forms the basis of information for healthcare professionals to use in order to administer and prescribe the drug in the correct way and with appropriate information required to guide a treatment decision. The risks associated with any particular drug can be managed by following the SmPC guidance. A summary of the typical contents of an SmPC is shown in Figure 1. The EMA define the SmPC functions as “Describing the properties and the officially approved conditions of use of a medicine” (EMA, 2017).
A number of clinical pharmacology support studies are required to successfully register small molecule drugs. These will be summarised in the following section.

Figure 1 – Typical structure and contents of an SmPC (EMA , 2017)
Clinical Pharmacology Support Studies
Absolute Bioavailability Study (BA)
Rationale and Objectives
Absolute bioavailability is sometimes referred to as absolute oral bioavailability (Fp.o.). These studies are carried out to determine how much of an investigational product is absorbed in the gastrointestinal system and metabolised in the body (Toutain and Bousquet-Melou, 2004). A determination of the quantity of the drug successfully enters the systemic circulation, and is therefore available to the target, can be made. This information is used to inform important assessments over investigational drug activity during the analysis of further pharmacokinetic (PK) data (FDA.gov, 2014).
In traditional studies, both intravenous (IV) and oral routes of administration are observed Toutain and Bousquet-Melou, 2004). These studies are often structured as ‘crossover studies’. Participants receive clinically relevant doses of both an oral and IV administration form (FDA.gov 2014), so that a characterisation of the PK profile of the product and any active metabolites can be made. These PKs are compared to determine the absolute oral bioavailability. If the drug formulation has been primarily prepared for oral use there may be an extensive re-formulation task required to produce an IV administrable drug that is both stable and sterile, This can be particularly difficult for investigational products that are not freely soluble and may be extremely challenging to re-formulate into an IV appropriate dosage form (ICH, 2009). Further complications surround the administration of a new drug through a route not previously studied as the only data available will be from animal toxicology studies (ICH, 2009). Figure 2 shows the equations used to determine absolute oral bioavailability.
Absolute Bioavailability (F) =
AUCoral
x
Doseiv
AUCiv
Doseoral
Figure 2 – Formula for calculating absolute bioavailability
Radio-label studies are a more modern approach, approved by licencing authorities. A radio-labelled 14C micro-dose is administered by IV alongside an oral dose form. Results are measured by liquid chromatography‐tandem mass spectrometry (LC‐MS/MS) or accelerator mass spectrometry (AMS). LC–MS/MS allows simultaneous detection of both drug administrations so, has cost and time benefits. However, for investigational products that have a particularly high volume of distribution AMS can provide a more specific lower limit of quantitation (Xu et al., 2014).
Design
To illustrate the design on a typical Absolute Bioavailability study, I will describe how this was conducted in 2014 for the drug, tasimelteon by Vanda Pharmaceuticals (ClinicalTrials.gov Identifier: NCT02130999) as this trial represents the conventional method for determining absolute bioavailability.
In this healthy volunteer crossover study, a single 20mg oral dose was compared to a 2mg IV infusion. 14 participants were randomised into two groups. One received the oral administration followed by a washout period and then received an IV administration while the second group received their dosing in the reverse order. Bioavailability was estimated from the geometric mean ratio (GMR) that was calculated from an analysis of variance (ANOVA) on the dose-corrected AUC0-inf. The study summary is provided in figure 3.

Figure 3 – Summary of Absolute Bioavailability study for tasimelteon. Adapted from (Clinicaltrials.gov, 2016)
Use of data
We can see from the Summary of Product Characteristics (SmPC) for Hetlioz™ that the absolute oral bioavailability is provided and listed as 38% with a peak blood plasma concentration time (Tmax) of 0.5hrs (EMA, n.d.). Other information in this section of the SmPC refers to food-effect which will be directly discussed later on.
Food-Drug Interaction Study
Rationale and Objectives
The EMA (2012) provide extensive guidance on food interaction studies. They describe the objective of this study as “minimising variability and obtaining optimal exposure”. Food can have a dramatic effect on the bioavailability of drugs administered orally. The biological response to feeding, for example pH changes as a result of acid secretion, changes in blood flow and gastric clearance rates can impact on drug absorption and metabolism (FDA.gov, 2002). Food can also affect drug BA as a direct result of an interaction between the food and the investigational products, most often due to chelation (Bushra, Aslam and Khan, 2011). In most cases, food-drug interaction studies are primarily focussed around the impact of food on drug exposure, absorption and metabolism.
Further interactions can occur as a result of metabolic pathways. Some foods such as, grapefruit are metabolised by the CYP3A4 enzyme, which is one of the most common metabolic routes for medications (Kirby and Unadkat, 2007). Foods can also inhibit other liver enzymes for example CYP2C9 in the case of cranberry (Yamreudeewong, et al., 1995).
The EMA (2012) state that the drug PK when taken with a high-fat meal must be determined. Depending on the investigational product’s solubility characteristics, it may be necessary to carry out further food-interaction studies investigate specific timing recommendations for dosing and if necessary, the effect with different food compositions. If the drug is advised to be dosed on an empty stomach, studies should be carried out to determine the sufficient fasting time period prior to dosing that should be achieved. If the investigational product is advised to be taken with food the appropriateness of the drug indication for paediatric groups should be considered.
Design
The FDA (2002) suggest a “randomized, balanced, single-dose, two-treatment (fed vs. fasting), two-period, two-sequence crossover design” in which one group receives a dosage in the unfed state and then after a washout period, receives a dosage following a meal. Meanwhile the second group will receive these doses in the reverse order.
The EMA (2012) suggests a quite detailed study design alongside the composition of the test meals which can be seen in figure 4.

Figure 4 – Extract from EMA guidance describing design of a food-interaction study. Adapted from (EMA, 2012).
Use of Data
Food effect data is used to make recommendations directly in the SmPC and are usually significantly important to the dosing of the drug. Prescribers should make patients aware of any and all food-effects especially as these are seen as being within the control of the patient to ensure correct, safe and appropriate dosing. If drug absorption or drug efficacy is decreased when taken with food, compared to in a fasted-state, drugs will be recommended to be taken on an empty stomach (EMA, 2012). The geometric mean ratios of Cmax and AUC must be between 80-125%, with 90% confidence in order for no food-effect to be determined (FDA, 2002).
Examples of these are given in figure 5, which shows an SmPC extract for warfarin, describing potentially dangerous food-effects due to interaction of certain foods on metabolic pathways while Figure 6 shows an SmPC extract for levothyroxine, explaining the requirement to take the drug in the fasted state.

Figure 5 – SmPC extract for warfarin, indicating food-effect. Adapted from (Medicines.org.uk, 2017)

Figure 6 – SmPC extract for levothyroxine drug Eltroxin, indicating food-effect. Adapted from (Medicines.org.uk, 2019a).
Mass Balance (ADME) Study
Rationale and Objectives
The mass balance study looks to determine the excretion and metabolism mechanisms of an investigational product and its metabolites using radio-labelled compounds. These studies are sometimes termed ‘human radio-label studies’. The drug is tagged with a radioactive marker and the concentration‐time profiles for plasma, whole blood and specific tissue concentration are determined. This allows for an assessment of the distribution of the investigational drug through the body. PK data (T1/2, Cmax, Tmax, AUC etc) can also be generated from these studies. The proportion of labelled material recovered in excreta is analysed to determine the elimination and metabolism of the investigational product. The principle is to attempt to recover 100% of the radiolabelled drug, however, this is likely impossible to achieve as a result of an inability to collect every molecule of excreta produced (Roffey et al., 2007).
Metabolic profiling is carried out by LC/MS/MS to provide confirmatory evidence to support findings from non-clinical animal toxicology studies. If metabolites are observed that were not present in the animal models, further toxicology studies may be required. If these studies are carried out at an early stage in drug development, information on metabolites and elimination can guide future for example, if the drug is shown to be renally eliminated, a renal impairment study may be required or special populations studies may be needed (Beaumont et al., 2014). Figure 7 shows a summary the concept behind the ADME radiolabel administration and detection.
Micro-tracer dosing for ADME studies in healthy participants followed by AMS, may be used as an alternative method if there are safety concerns or a very small pharmacologically active dose range, or if greater precision is required (Lozac'h et al., 2018).

Figure 7 – Summary of principle of ADME study. Adapted from (Stypinksi, 2015).
Design
A 2011 study conducted by US WorldMeds LLC (ClinicalTrials.gov Identifier: NCT01310296) outlines a study design involving 12 participants. In this cross-over study participants were randomised into two groups where they received a C14-labelled oral solution of lofexidine. Plasma and excreta samples were collected for 216 hours. This study also looked to determine bioavailability so, included a second arm where participants received an IV dosage of the drug. Figure 8 shows an extract of this study design.

Figure 8 – Summary of ADME study design for lofexidine. Adapted from (Clinicaltrials.gov, 2017a).
Use of Data
The ADME study provides context for analysis of data collected when investigating the metabolic enzyme routes. They suggest interaction studies be carried out with enzyme inhibitors or pharmacogenetic studies to further elucidate this area. Active metabolites can be identified through this study. If the level of protein binding is found to be high, further protein interaction studies may also be recommended (EMA, 2012). As such, it does not directly lead to prescribing statements in the SmPC but, instead contributes to the analysis of other data gathered in additional studies.
Thorough QT Study
Rationale and Objectives
A delay in the QT interval can lead to cardiac arrhythmia and may lead to torsade de points, a phenomenon which in turn, can lead to ventricular fibrillation and death as well as other problematic events such as, tachyarrhythmia. Drugs can prolong the QT interval and therefore, increase the risk of the development of cardiac problems. A thorough QT/QTc study evaluates the drug effect on cardiac action by monitoring with an electrocardiogram.
Ultimately, the thorough QT/QTc study determines if the investigational product has an effect of cardiac repolarisation though the monitoring of the QT interval. If the results of this investigative work show an impact on the QT interval, an expanded safety evaluation will need to be carried out (ICH, 2005).
Design
The design of the thorough QT study is given in some detail by ICH E14 regulation. This is described as requiring “[randomisation, blinding] and a concurrent placebo group”. Both parallel and crossover designs are acceptable (ICH, 2005). Figure 9 shows an extract from the ICH guidelines describing the study design.
The ICH requires that dose-response and concentration-response relationship with the QT interval prolongation are determined. They suggest that investigations are carried to exceed the anticipated therapeutic dose, provided adverse effects are not severe enough to make this untenable.

Figure 9 – Extract from ICH E14 guidelines, describing thorough QT study design. Adapted from (ICH, 2005)
Use of Data
The data collected from the thorough QT study informs the decision-making process for further investigations. If QT interval prolongation is observed, this must be further investigated in comparison to other drugs of the same class. If the positive result is 5ms or less, this would not necessarily increase the chance of torsade de points. Drugs that increase the interval by 20ms or more are characterised as “substantially” increasing the chance of proarrhymia.
The ICH further recommended some specific labelling to highlight this risk to prescribers this is shown in figure 10 while figure 11 shows an extract from an SmPC for the fluconazole drug, Diflucan, which demonstrates how QT interval prolongation is referenced and influences on prescribing decisions in the SmPC.
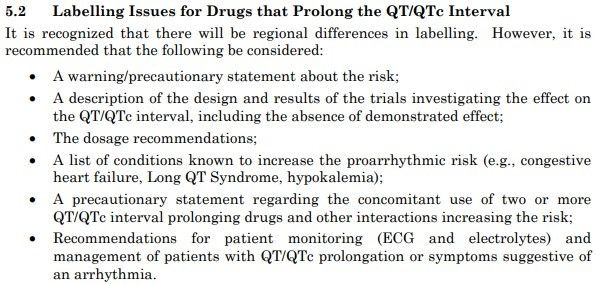
Figure 10 – Summary of labelling considerations for QT prolongation. Adapted from (ICH, 2005)

Figure 11 – Extract from SmPC of fluconazole to demonstrate QT prolongation impact on prescribing decisions. Adapted from (Medicines.org.uk, 2019b)
Renal Impairment Study
Rationale and Objectives
A renal impairment study is recommended by the FDA Draft Guidance (2002) if the investigational product, or its metabolites are cleared through the renal or biliary routes. This is because poor renal function can impact on metabolic pathways in both the liver and GI tract. Renal impairment studies are further suggested for any chronically administered drugs. As such, it is commonplace that some kind of renal assessment is carried out. The depth of the investigation is led by assessments made during indicative studies (FDA, 2002).
Design
Renal impairment studies can begin with a reduced PK Study followed by a full PK Study. If the product elimination is likely to impact on dialysis, an assessment of this may also be required.
In the reduced PK study, patients with end-stage renal disease, who have not yet commenced dialysis treatment, have their unbound drug plasma or whole-blood PK data from a single-dose administration, compared to those who have no impairment (control groups should consist of patients without renal impairment who are otherwise healthy). An assessment is then made to determine any significant difference between these patients’ function that might infer the need to alter the prescribing advice. If this is seen, a full PK study should then be completed (FDA, 2002).
In the full PK study, the same control group from the reduced study should be used. This study is aiming to estimate the creatine clearance rate (CLcr) or glomerular filtration rate (eGFR). While the eGFR method tends to be the new standard measure, both CLcr and eGFR values must be given. eGFR is calculation via the Modification of diet in renal disease (MDRD) method. CLcr is calculated from the Cockcroft-Gault equation (FDA, 2002). These are shown below.

The effect of dialysis assessment only needs to be completed where dialysis results is significant drug elimination, or where the investigational product is likely to impact on the efficacy of dialysis (FDA, 2002).
A clinical trial extract for a renal impairment study on the drug plerixafor (ClinicalTrials.gov Identifier: NCT00445302) is shown in figure 12.

Figure 12 – Renal impairment study design of plerixafor. Adapted from (Clinicaltrials.gov, 2014a).
Use of Data
Participants with eGFR reduction in the range of 60-89 mL/min/1.73m2 with no renal impairment are not considered to be at any greater risk of problems from renally eliminated products.
Dosages should be reduced by half for those a creatinine clearance of 30-59 mL/min or eGFR of 30-59 mL/min/1.73 m2 (FDA, 2002).
An SmPC extract for a plerixafor drug, Mozobil is shown in figure 13 to demonstrate how this information translates into prescribing guidance.

Figure 13 – SmPC extract for Mozobil. Adapted from (Medicines.org.uk, 2019c).
Hepatic Impairment Study
Rationale and Objectives
The rationale behind the hepatic impairment study is very similar to that of the renal impairment study. Many drugs are metabolised by the liver and so, individuals who have some kind of hepatic impairment may require modification of the prescribing guidance. The FDA (2003) specifically recommend hepatic impairment studies be undertaken if over 20% of the metabolism or elimination of a drug is through the hepatic pathway or, if there is evidence of a narrow therapeutic range and the liver is involved in the metabolism and clearance of a drug at all.
Analyses of PK studies in patients with hepatic impairment have shown a negative correlation between drug elimination and hepatic impairment.
Design
A full study design is suggested by the FDA (2003) in order to define the dose range across all severities of hepatic impairment. Multiple dosing is recommended at the planned clinical level although, this may be altered if there is safety concern for those with hepatic impairment in order to reach steady state 3 arms (each with 6 or more patients) should be run for each of the Child-Pugh categorisation (mild, moderate and severe). Control groups should be from the patient population. A reduced study design would only involve patients who score moderate on the Child-Pugh scale and results would be applied to those in the mild category. Any patients classed as severe would eb contraindicated.
Population PK methods are also suggested in order to give insight into the potential effect of hepatic impairment. In this case patients in Phase II and III studies are to be assessed against measurements of hepatic function when administered with the drug. This analysis must be pre-planned and determine the severity of hepatic disease. It must also be carried out in a representative sample of the range of impairment.
An extract of the non-randomised, single-dose hepatic impairment study into deflazacort (ClinicalTrials.gov Identifier: NCT02286609) is shown in figure 14 below

Figure 14 – summary of hepatic impairment study design in deflazacort. Adapted from (Clinicaltrials.gov, 2017b).
Use of Data
PK data collected should be analysed to determine AUC, Cmax, CL/F, Renal and non-renal clearance, volume of distribution and half-life. Modelling is the carried out to determine how hepatic impairment impacts on these measurements and prescribing recommendations are made on that basis.
An SmPC extract for deflazacort is shown below in figure 15 to demonstrate how these impairment studies affect prescribing information.
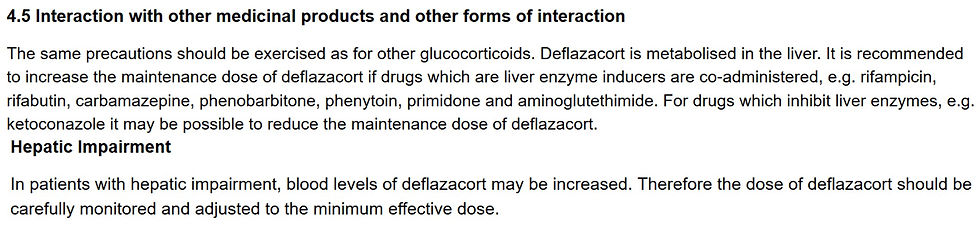
Figure 15 – extract from Calcort SmPC to demonstrate prescribing advice regarding renal impairment. Adapted from (Medicines.org.uk, 2019d).
Drug-drug Interaction (DDI) Studies
Rationale and objectives
DDIs are described as “a clinically significant alteration in the effect of one drug as a consequence of coadministration of another” (Hines and Murphy, 2011). They can lead to severe side effects and are one of the major causes of product licence withdrawal (Yu et al., 2014) and often result in significant patient effects as a result of toxicity or lack of efficacy where drug products are metabolised by the same pathways. DDIs are of additional concern when considering older patients who, are likely to be subject to co-morbidities (suffering from multiple chronic conditions) as and as such, be prescribed a number of medication regimens (Johnell and Fastbom, 2012). Both the EMA and FDA suggest in-vitro and in-vivo studies of different transporters used by active drugs and their metabolites. as well as the use of modelling to predict likely interactions (Prueksaritanont et al., 2013).
The EMA (2012) state that if an interaction is observed in-vitro and in-vivo tests must be carried out in order to determine the interaction mechanism.
Design
The FDA (2012) guidance states that DDI studies must be carried out if drug products are classified as substrates, inhibitors or inducers of major cytochrome P450 or Glucuronosyltransferase enzymes. These studies must use human liver tissue. in-vitro studies are carried out first, to determine intrinsic clearance with and without an inhibitor or inducer. In-vivo studies are then required if activity is shown.
Transporter-mediated interaction must also be characterised and the FDA guidance outlines a number of transporters that investigational products must be screened against. Comparative PK data from participants with heterogenous enzyme genotypes can also be used to asses the likelihood of enzyme interaction on drug metabolism (Yu et al., 2014).
The FDA 2017 draft guidance states that Population PK in-silico models are acceptable studies if interactions are thought to be minimal (FDA, 2017). EMA (2012) outline the acceptability of Population PK analysis if normal DDI studies cannot be performed.
Figure 16 shows the typical design for a DDI study of the progesterone receptor modulator, Proellex® (ClinicalTrials.gov Identifier: NCT00741468) using enzyme probes to determine interactions.

Figure 16 – Extract of DDI clinical trial in Proellex® demonstrating DDI trial design. Adapted from (Clinicaltrials.gov, 2014b)
Use of Data
Where drug interactions are observed prescribing advice is modified. In exposure studies a 2-fold change usually results in dosing recommendations being altered (Yu et al., 2014). Figure 17 shows an SmPC extract for Digoxin, it shows only some of the DDIs as for this drug, there are over 12 interaction areas, each featuring multiple drugs. The extract provided is therefore indicative of the kind of prescribing advice provided.

Figure 17 - Modified extract form digoxin SmPC demonstrating drug interaction guidance. Adapted from (Medicines.org.uk, 2019e).
Population PK
Rationale and Objectives
Population PK describes a model which can characterise drug PK and explain variability in subjects. It integrates PK data from a range of sources to simulate exposure, dosing regiments and individual PK parameters that can be used in later assessments in dose-response (Dykstra et al., 2015). The FDA (2019) draft guidance provides a range of used for Population PK analysis, while this is only in draft, it demonstrates the strong support population PK analysis methods receive form the regulatory agencies.
“Selecting Dosing Regimens for Clinical Trials. Deriving Sample Size and Sampling Scheme Requirements. Deriving Exposure Metrics for Exposure-Response Analysis. [Paediatric] Study Designs. Specific Population [PK property descriptions]. Drug-Drug Interactions. [Simulations of:] Fixed-Effect Estimates Between-Subject Variability” (FDA.gov, 2019).
There is growing interested in the use of Population PK modelling, especially when carrying out conventional clinical testing on specific target populations is difficult (Johnson and Rostami-Hodjegan, 2011).
Design
Population PK model designs are not described in the guidelines. However, A description of the model, how it was built, applied and validated is required. In a study looking at mycophenolic acid and tacrolimus administration post renal transplantation the following design was used.
Non-linear mixed-effect modelling performed by using specialist analytical software. PK data was estimated by this software. Inter-participant variability was determined by use of a second model and mixed-error models were used to determine any residual error. Model validity was tested by a comparison of these data with actual measured PK values (Musuamba et al., 2012).
Use of Data
The use of Population PK data in drug development is extensive and increasing as model sophistication improves and regulatory acceptance grows. To that end it is difficult to say how the use of Population PK modelling directly influences prescribing information as the use of the Population PK model is likely to be different for each investigational drug product (Jamei, 2016).
Bioequivalence Study (BE)
Rationale and Objectives
While not required for the licensing of new chemical entities, bioequivalence is a very important principle to demonstrate for the licensing of generics and additional drug formulations.
BE studies are carried out to determine the efficacy of a drug in different formulations. BE aims to show that these different formulations are equally efficacious and elicit a comparable drug-response. BE is determined by the AUC and the maximum blood-plasma concentration (Cmax). BE also becomes important under the USA’s Drug Price Competition and Patent Term Restoration Act, following the expiration of drug patents, generic versions should be made available for general use. These generic drugs must also demonstrate BE after being administered in the same quantities, under similar conditions (Chow, 2014).
Design
To illustrate the designs of typical BE studies, I will consider a BE study of different sildenafil formulations. A 2012 study by Pfizer (ClinicalTrials.gov Identifier: NCT01737203) looked to determine BE for a 50mg orally disintegrating tablet taken both with and without water were compared to the conventional 50mg oral tablet formulation. In this study, 53 participants were randomised in a crossover design. A summary of this shown in figure 18. In this study AUC0-inf was measured alongside Cmax. These data are then be used to determine BE.

Figure 18 - Summary of Bioequivalence study for sildenafil. Adapted from (Clinicaltrials.gov, 2012).
Use of Data
This BE PK data is used in the SmPC to direct appropriate dosing. When we compare the SmPC for Pfizer produced, Viagra® against the generic produced by Sigma Pharmaceuticals PLC we see that the PK data is, in fact identical (see figure 19) and prescribing statements in each SmPC are the same. This reflects both products demonstrate BE and so, they can be used in exactly the same manner.

Figure 19 – SmPC extracts from Viagra® and sildenafil generic. Adapted from (Medicines.org.uk, 2018 & 2019f)
References
Beaumont, C., Young, G., Cavalier, T. and Young, M. (2014). Human absorption, distribution, metabolism and excretion properties of drug molecules: a plethora of approaches. British Journal of Clinical Pharmacology, 78(6), pp.1185-1200.
Bushra, R., Aslam, N. and Khan, A. (2011). Food Drug Interactions. Oman Medical Journal, 26(2), pp.77-83.
Chow, S. (2014). Bioavailability and bioequivalence in drug development. Wiley Interdisciplinary Reviews: Computational Statistics, 6(4), pp.304-312.
Clinicaltrials.gov. (2012). Bioequivalence Study For Orally-Disintegrating Tablet Of Sildenafil - Full Text View - ClinicalTrials.gov. [online] Available at: https://clinicaltrials.gov/ct2/show/NCT01737203 [Accessed 26 Oct. 2019].
Clinicaltrials.gov. (2014). Safety, Pharmacokinetics (PK), And Hematological Activity Of AMD3100 (Plerixafor) In Subjects With Renal Impairment - Full Text View - ClinicalTrials.gov. [online] Available at: https://clinicaltrials.gov/ct2/show/NCT00445302 [Accessed 30 Oct. 2019].
Clinicaltrials.gov. (2014b). Open-Label, Multiple-Dose, Non-Randomized Study to Assess Drug-Drug Interactions of Proellex® in Female Subjects - Full Text View - ClinicalTrials.gov. [online] Available at: https://clinicaltrials.gov/ct2/show/NCT00741468 [Accessed 30 Oct. 2019].
Clinicaltrials.gov. (2016). Open Label Study to Assess the Absolute Bioavailability of Tasimelteon (HETLIOZ™) - Full Text View - ClinicalTrials.gov. [online] Available at: https://clinicaltrials.gov/ct2/show/NCT02130999 [Accessed 26 Oct. 2019].
Clinicaltrials.gov. (2017a). Lofexidine ADME & Mass Balance in Volunteers - Full Text View - ClinicalTrials.gov. [online] Available at: https://clinicaltrials.gov/ct2/show/NCT01310296 [Accessed 27 Oct. 2019].
Clinicaltrials.gov. (2017b). A Single Dose Evaluation of the Effects of Moderate Hepatic Impairment on Deflazacort Pharmacokinetics - Full Text View - ClinicalTrials.gov. [online] Available at: https://clinicaltrials.gov/ct2/show/NCT02286609 [Accessed 31 Oct. 2019].
Dykstra, K., Mehrotra, N., Tornøe, C., Kastrissios, H., Patel, B., Al-Huniti, N., Jadhav, P., Wang, Y. and Byon, W. (2015). Reporting guidelines for population pharmacokinetic analyses. Journal of Pharmacokinetics and Pharmacodynamics, 42(3), pp.301-314.
EMA (2017). Summary of product characteristics (SmPC) - What is it and what does it contain?. https://www.ema.europa.eu/documents/presentation/presentation-summary-product-characteristics-smpc_en.pdf [Accessed 32 Oct. 2019]
EMA (n.d.). Hetlioz, INN. ANNEX I - SUMMARY OF PRODUCT CHARACTERISTICS. [online] Available at: https://ec.europa.eu/health/documents/community-register/2015/20150703132093/anx_132093_en.pdf [Accessed 22 Oct. 2019].
EMA. (2012). Guideline on the investigation of drug interactions. [online] Available at: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-investigation-drug-interactions_en.pdf [Accessed 27 Oct. 2019].
EMA. (2015). SUMMARY OF PRODUCT CHARACTERISTICS - HETLIOZ 20 mg hard capsules. [online] Available at: https://ec.europa.eu/health/documents/community-register/2015/20150703132093/anx_132093_en.pdf [Accessed 26 Oct. 2019].
FDA. (2003). Pharmacokinetics in Patients with Impaired Hepatic Function: Study Des. [online] Available at: https://www.fda.gov/media/71311 [Accessed 31 Oct. 2019].
FDA.gov. (2002). Food-Effect Bioavailability and Fed Bioequivalence Studies | FDA. [online] Available at: https://www.fda.gov/media/70945 [Accessed 31 Oct. 2019].
FDA.gov. (2014). Bioavailability and Bioequivalence Studies Submitted in NDAs or INDs — General Considerations | FDA. [online] Available at: https://www.fda.gov/media/88254 [Accessed 31 Oct. 2019].
FDA.gov. (2017). Clinical Drug Interaction Studies — Study Design, Data Analysis, and Clinical Implications Guidance for Industry | FDA. [online] Available at: https://www.fda.gov/media/82734 [Accessed 31 Oct. 2019].
FDA.gov. (2019). Population Pharmacokinetics - Guidance for Industry. [online] Available at: https://www.fda.gov/media/128793/download [Accessed 31 Oct. 2019].
Hines, L. and Murphy, J. (2011). Potentially Harmful Drug–Drug Interactions in the Elderly: A Review. The American Journal of Geriatric Pharmacotherapy, 9(6), pp.364-377.
ICH. (2005). THE CLINICAL EVALUATION OF QT/QTC INTERVAL PROLONGATION AND PROARRHYTHMIC POTENTIAL FOR NONANTIARRHYTHMIC DRUGS E14. [online] Available at: https://database.ich.org/sites/default/files/E14_Guideline.pdf [Accessed 28 Oct. 2019].
ICH. (2009). GUIDANCE ON NONCLINICAL SAFETY STUDIES FOR THE CONDUCT OF HUMAN CLINICAL TRIALS AND MARKETING AUTHORIZATION FOR PHARMACEUTICALS M3 (R2). [online] Available at: https://database.ich.org/sites/default/files/M3_R2__Guideline.pdf [Accessed 27 Oct. 2019].
Jamei, M. (2016). Recent Advances in Development and Application of Physiologically-Based Pharmacokinetic (PBPK) Models: a Transition from Academic Curiosity to Regulatory Acceptance. Current Pharmacology Reports, 2(3), pp.161-169.
Johnell, K. and Fastbom, J. (2012). Comparison of Prescription Drug Use between Community-Dwelling and Institutionalized Elderly in Sweden. Drugs & Aging, 29(9), pp.751-758.
Johnson, T. and Rostami-Hodjegan, A. (2011). Resurgence in the use of physiologically based pharmacokinetic models in pediatric clinical pharmacology: parallel shift in incorporating the knowledge of biological elements and increased applicability to drug development and clinical practice. Pediatric Anesthesia, 21(3), pp.291-301.
Kirby, B. and Unadkat, J. (2007). Grapefruit Juice, a Glass Full of Drug Interactions?. Clinical Pharmacology & Therapeutics, 81(5), pp.631-633.
Lozac'h, F., Fahrni, S., Maria, D., Welte, C., Bourquin, J., Synal, H., Pearson, D., Walles, M. and Camenisch, G. (2018). Evaluation of cAMS for14C microtracer ADME studies: opportunities to change the current drug development paradigm. Bioanalysis, 10(5), pp.321-339.
Medicines.org.uk. (2017). Warfarin 1 mg Tablets - Patient Information Leaflet (PIL) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/9472https://www.medicines.org.uk/emc/product/4442/pil [Accessed 27 Oct. 2019].
Medicines.org.uk. (2018). Sildenafil 50 mg film-coated tablets - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/9472 [Accessed 26 Oct. 2019].
Medicines.org.uk. (2019a). Eltroxin 50 mcg tablets - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/434/smpc [Accessed 27 Oct. 2019].
Medicines.org.uk. (2019b). Diflucan 150 Capsules - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/1065/ [Accessed 31 Oct. 2019].
Medicines.org.uk. (2019c). Mozobil 20 mg/ml solution for injection - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/790 [Accessed 30 Oct. 2019].
Medicines.org.uk. (2019d). Calcort 6mg Tablets - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/6287 [Accessed 31 Oct. 2019].
Medicines.org.uk. (2019e). Digoxin Tablets BP 250 micrograms - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/5773 [Accessed 31 Oct. 2019].
Medicines.org.uk. (2019f). Sildenafil 25mg, 50mg, 100mg film-coated tablets - Summary of Product Characteristics (SmPC) - (emc). [online] Available at: https://www.medicines.org.uk/emc/product/3172 [Accessed 26 Oct. 2019].
Musuamba, F., Mourad, M., Haufroid, V., Demeyer, M., Capron, A., Delattre, I., Delaruelle, F., Wallemacq, P. and Verbeeck, R. (2012). A Simultaneous D-Optimal Designed Study for Population Pharmacokinetic Analyses of Mycophenolic Acid and Tacrolimus Early After Renal Transplantation. The Journal of Clinical Pharmacology, 52(12), pp.1833-1843.
Prueksaritanont, T., Chu, X., Gibson, C., Cui, D., Yee, K., Ballard, J., Cabalu, T. and Hochman, J. (2013). Drug–Drug Interaction Studies: Regulatory Guidance and An Industry Perspective. The AAPS Journal, 15(3), pp.629-645.
Roffey, S., Obach, R., Gedge, J. and Smith, D. (2007). What is the Objective of the Mass Balance Study? A Retrospective Analysis of Data in Animal and Human Excretion Studies Employing Radiolabeled Drugs. Drug Metabolism Reviews, 39(1), pp.17-43.
Stypinksi, D. (2015). Human ADME Study Design Considerations in Healthy Subjects and in Patients. [online] Celerion Applied Translational Medicine. Available at: https://www.celerion.com/wp-content/uploads/2015/11/Celerion_2015-San-Mateo-San-Diego-Clinical-Discussion-Forums_Human-ADME-Study-Design-Considerations.pdf [Accessed 27 Oct. 2019].
TOUTAIN, P. and BOUSQUET-MELOU, A. (2004). Bioavailability and its assessment. Journal of Veterinary Pharmacology and Therapeutics, 27(6), pp.455-466.
Xu, X., Jiang, H., Christopher, L., Shen, J., Zeng, J. and Arnold, M. (2014). Sensitivity-based analytical approaches to support human absolute bioavailability studies. Bioanalysis, 6(4), pp.497-504.
Yamreudeewong W, Henann NE, Fazio A, Lower DL, Cassidy TG. Drug-food interactions in clinical practice. J Fam Pract 1995. Apr;40(4):376-384.
Yu, J., Ritchie, T., Mulgaonkar, A. and Ragueneau-Majlessi, I. (2014). Drug Disposition and Drug-Drug Interaction Data in 2013 FDA New Drug Applications: A Systematic Review. Drug Metabolism and Disposition, 42(12), pp.1991-2001.
An assignment by: Darren Wogman MSc. Completed as part of Pharmaceutical Medicine MSc at King's College London


コメント